Osteoarthritis is the most common type of arthritis. It’s basically the wearing away of the cartilage caps the bones in our joints. Arthritis itself is the swelling and tenderness of our joints. The main symptoms are joint pains, discomfort, swelling, decreased motion, and stiffness. Some of the risk factors for arthritis include age, sex, family history, previous injuries, obesity, and more. There are numerous ways of treating these issues, with us getting more and more sophisticated ones almost by the day. Of course, it’s best to prevent arthritis in the first place. This can be done by maintaining good weight, regular physical activities, wearing appropriate footwear, using ergonomic aids at home, and more.
Want to learn more? Keep reading the article by Dr. Jocelyne Melchior-Capiot!
In January 2000, the United Nations declared the first decade of the third millennium to be the decade of bone and joint diseases. Of these, osteoarthritis is the disease that causes the most pain and functional impairment worldwide.
What is osteoarthritis?
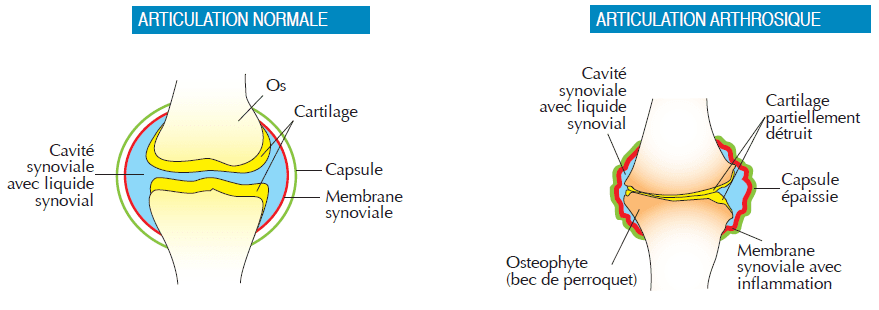
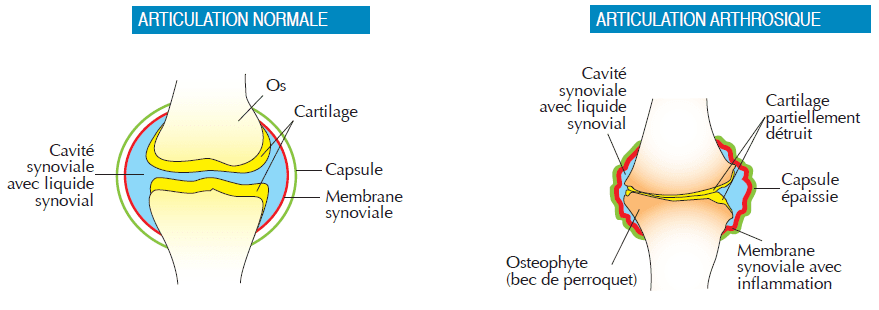
Osteoarthritis is the most common joint disease in the Western world and is caused by the progressive deterioration of cartilage over time, which then spreads to all the structures of the joint, including the bone and synovial tissue.
Cartilage, a strong, elastic tissue, lines the ends of the bones and allows the joint surfaces to slide freely over each other during movement.
In osteoarthritis, the cartilage gradually deteriorates and loses its original qualities, i.e. its flexibility and elasticity. Microfissures appear and grow. In addition, the quality of the synovial fluid, a viscous and clear liquid like egg white, which normally lubricates the joint, is altered. With time, an inflammation develops which tends to become chronic and recurrent, accompanied by pain.
As wear progresses, the cartilage can sometimes disappear completely in certain joint areas, generating new biomechanical constraints, following which bony outgrowths (“parrot’s beak”) can appear, further accentuating the painful phenomena and the muscular compensation phenomena.
Which joints are affected by osteoarthritis?
All joints can be affected by osteoarthritis. Most often it is the hips, knees, hands, and spine that are affected.
What are the causes?
- overweight (especially for osteoarthritis of the hips and knees)
- heredity (for nodular osteoarthritis of the fingers)
- age
- a history of trauma or overuse of a joint (intensive sports activities, demanding jobs) – defects in the axis of the lower limbs (X-shaped knees)
- another disease affecting the joints (rheumatoid arthritis, gout, chondrocalcinosis, disease of the tendons, ablation of a meniscus, etc. )
How common is osteoarthritis?
Osteoarthritis occurs in almost all people after the age of 50. In France, it affects 65% of people over the age of 65. However, its expressiveness and repercussions vary greatly from one person to another.
The symptoms and evolution of osteoarthritis
Osteoarthritis frequently manifests itself by pain and/or joint stiffness which increases after effort and is sometimes associated with local swelling. The pain often subsides with rest.
Sometimes, against a background of stiffness and limited mobility, iterative painful attacks with effusion (congestive osteoarthritis) may be more acute.
Osteoarthritis generally progresses very slowly. Sometimes more than 20 years may pass between the first injury to the cartilage and the onset of pain in the joint. Over time, deformities may develop in the affected joints (e.g. nodules in the fingers).
How is osteoarthritis diagnosed?
The doctor suspects osteoarthritis on the basis of simple elements found during questioning and clinical examination. He confirms his diagnosis and assesses the severity of the damage by means of simple complementary examinations such as X-rays. The use of more sophisticated examinations such as CT scans or MRI (magnetic resonance imaging) may subsequently prove useful. A blood test and/or a puncture of the joint may be necessary to rule out another cause of joint pain.
There is currently no cure for osteoarthritis, but it is possible to slow down its progression. Several simple measures can alleviate the pain and allow a better quality of life. The first step is to offer the patient advice on simple non-medicinal approaches such as exercise and weight loss and to empower them to take an active role in their treatment. The combination with drug treatment is decided in collaboration with the patient to define the optimal management according to the site and severity of the osteoarthritis.
Medicinal treatments
- Often indispensable, analgesics are used, sometimes on a daily basis, to combat pain. Paracetamol is the basic medication, with little toxicity for the digestive tract at the recommended doses (1 to 3-4 grams/day for an adult).
- Aspirin or non-steroidal anti-inflammatory drugs (NSAIDs) are effective for pain and inflammation. However, taken as self-medication, their toxicity for the digestive tract makes them dangerous in case of a history of digestive tract ulcer. They are frequently combined with stomach-protecting drugs to reduce stomach toxicity. Topical anti-inflammatory drugs (cream, gel, plaster) are often very useful.
- When the previous drugs are no longer effective, more powerful molecules can be prescribed by the doctor: morphine derivatives, taken orally or transcutaneously (patches).
- Cortisone, taken orally or as an intra-articular infiltration, is also sometimes used. Given the side effects it can cause, its use requires strict medical supervision.
Non-medicinal treatments
The local application of heat to the skin of a painful joint often leads to an improvement in pain. In some patients with osteoarthritis and effusion, the application of cold will be the most appreciated.
Physiotherapy is essential to reduce pain and maintain mobility. With the help of the physiotherapist, a personalized rehabilitation program is set up. Physical activity should be maintained as it helps to alleviate painful symptoms and maintain a healthy body weight, which reduces the strain on the diseased joints. In addition, exercise improves general well-being.
Moderate stretching will keep muscles and tendons supple and strong, while low-impact exercise (cycling, swimming, water aerobics) can reduce pain and maintain joint mobility. Thermal cures are also very beneficial for patients with osteoarthritis in several places (polyarthritis).
Technical aids can, especially in elderly patients, help to reduce pain and improve safety, autonomy, and quality of life. These include
- various types of canes (in the hand opposite the painful joint)
- resting splints, supporting orthoses – grippers (for picking up objects from the floor or shelves)
- tools suitable for opening cans and jars
- toilet seat raisers
- wall grab bars
When medical treatment is no longer able to reduce the patient’s pain, a surgical solution should be considered. Several options are possible: arthroscopy with the cleaning of the arthritic joint, correction of defects in the axes of the lower limbs (osteotomies), blocking of a joint with screws (arthrodesis), fitting of a joint prosthesis.
More recent treatment modalities
- Chondroprotection:
Encouraging results in slowing the progression of osteoarthritis have been obtained with chondroitin sulfate and glucosamine sulfate. These drugs, known as slow-acting symptomatic drugs, are well tolerated and also have an effect on painful symptoms, but their effectiveness is only apparent after several weeks of use. They are a basic treatment for osteoarthritis.
- Viscosupplementation:
This is a technique that consists of injecting a viscous, transparent gel made of hyaluronic acid into the joint affected by osteoarthritis. This substance, which is naturally present in the body’s tissues and in the joint fluid, lubricates the cartilage, has a “cushioning” effect, and thus promotes greater mobility while reducing painful symptoms. A series of at least 3 injections are given, once a week. The analgesic effect obtained can last for several months. If necessary, a further series of injections can be given later.
- Pulsed Signal Therapy (PST): A new approach to physical medicine, patented in the United States, Pulsed Signal Therapy is a powerful analgesic technique based on the combined action of an electric and magnetic current. A pulsed signal, transmitted to the painful area of the musculoskeletal system, will develop both an analgesic and anti-inflammatory effect as well as an improvement of the local tissue quality. A series of 9 to 12 one-hour sessions is necessary to obtain this analgesic and anti-inflammatory effect, which can last for several months. For the time being, this innovative treatment, practised only by a dozen or so doctors in Switzerland, is covered by certain supplementary insurance companies.
- New therapeutic research: Platelet-enriched plasma injections: a technique widely used in sports medicine, it consists of taking a small amount of the patient’s blood, centrifuging it to separate its various components; the red and white blood cells are removed and the platelet-enriched plasma is then reinjected into the area to be treated. The platelets synthesise substances with anti-inflammatory and healing properties. A study on a small number of patients in knee osteoarthritis shows encouraging medium-term results in terms of pain and slowing down the progression of osteoarthritis lesions in the joints assessed by MRI.
Stem cells: since 2012, a European team at the Montpellier University Hospital has been conducting a study to evaluate the effectiveness of injecting stem cells (obtained from fat cells) into joints affected by osteoarthritis, hoping to activate the ‘regeneration of damaged cartilage. Results are expected from 2016 to 2020.
Numerous pharmacological studies are underway to develop effective drugs for osteoarthritis: antigen F (tanezumab), zoledronic acid, strontium ranelate are being evaluated.
Preventing osteoarthritis? a few tips…
- maintain a healthy weight
- practice regular physical activity (walking, cycling, swimming, tai chi…).
- take care of your joints during sports activities, respect your pain, take breaks… In the event of significant pain, avoid overtaxing the joint.
- wear good walking shoes
- use ergonomic aids and possibly adapt your home with the help of an occupational therapist
- be an active participant in your treatment with your doctor










