Having elevated blood glucose levels could directly affect your vision. Furthermore, diabetes is the main cause of blindness from ages 20 to 74. Its impact on our vision can quite differ depending on the severity of the issue. Some people’s visions get blurry, some get glaucoma and yet some lose their ability to see entirely. Thankfully, we’re getting more and more treatment options as time inevitably moves on. The most effective weapon against it, however, is still prevention. If you experience any of these symptoms, it would be in your best interest to consult a doctor!
If you want to learn more, keep reading the article from Pr. Marc D. de Smet.
Increasing numbers of people have elevated blood glucose levels. If this condition persists, worsens or gets out of control, it can have consequences for vision. What can be done to prevent this additional complication? Should one go to the doctor more often? What measures should be taken if vision is already impaired? We will deal with these topics in this article.
The eye is a tiny camera that allows us to see the world around us. When the sun is shining, our vision stretches from the heights of the Aletsch glacier to the forests of the Jura. We see the movements of the climbers who want to conquer the Eiger as well as the small print for the renewal of our mortgage. The eye adapts to all these situations and seems to know its importance, for vision remains intact for the time being despite repeated spikes in blood sugar. However, this should not lead us to wrong conclusions, because diabetes does affect the eyes, but the latter adapt to maintain vision for years despite elevated blood sugar levels. Sugar is nevertheless a vital element and necessary for the proper functioning of the brain and eyes. It is not sugar per se that is problematic, but its consumption in excess – when there is too much sugar in the blood, it alters the function and survival of cells. The sophisticated functions that enable us to see are gradually disrupted. The way this loss of function manifests itself depends on the age of the patient and the duration of the diabetes.
Young people usually suffer from type I diabetes. The loss of vision takes place aggressively and explosively and is associated with bleeding inside the eye. Too high blood sugar destroys the capillaries, small vessels that are responsible for supplying oxygen to the retina. As a result, the retina, which is undersupplied with oxygen, produces factors that lead to the formation of new vessels. However, these are less resistant and more prone to bleeding. They are also the reason for the detachment of the retina and in some cases lead to blindness. Such serious concomitant diseases only develop after diabetes has been poorly controlled for more than 10 years, but every year counts. The better the control, the greater the chances of avoiding this complication.
The situation is different for older people with type II diabetes. If blood sugar cannot be brought under control over a period of 5 to 10 years, especially in combination with high blood pressure and increased cholesterol, the macula in particular is affected by a loss of function. This part of the eye (which we dealt with earlier) enables us to read and recognise faces. Here, the sugar changes the function of the retina itself. Instead of maintaining a compact shape, it enlarges and fills with water that it can no longer excrete. The larger this oedema becomes, the more difficult it becomes to reading and eventually the affected person can only recognise blurred shapes and can no longer read at all. If the oedema persists, the retina loses its shape, the scaffolding of the retina formed by Müller cells crumbles, the cells die and the oedema becomes permanent. From the fifth year after the onset of type II diabetes, the eye may need medical treatment.
But fortunately, the situation is not hopeless. Our arsenal of treatments is increasing every year. We understand more and more the possible courses of action at different stages of the disease, but our most effective weapon is prevention, closely followed by early detection. As part of prevention, we recommend appropriate monitoring by a general practitioner or a diabetologist. These professionals can prescribe treatment that lowers blood glucose and keeps it at an acceptable level. They can also treat the risk factors that can aggravate diabetes, if necessary. As part of early detection, an ophthalmologist can be seen regularly, even before vision actually deteriorates. There are many signs that are not visible to the patient but can be detected by the trained eye of a specialist. Some of these signs require no consequences, others may prompt him to begin proactive treatment. The earlier one acts, the better the outcome.
In recent years, technology has made ophthalmologists’ jobs much easier. Measuring vision remains important because it is a precious commodity for all of us to depend on. However, therapeutic decisions are now made with the help of highly accurate imaging techniques. A simple image of the back of the eye, preferably in colour, may initially be sufficient for early detection (Figure 1). It can be analysed by computer or examined by a specialist to detect signs of disease that require a more in-depth examination. A non-invasive technique called optical coherence tomography (OCT) can be used to examine the different layers of the retina, as well as the severity of inflammation and macular oedema (Figure 2). It can even help in planning therapy. In addition, angiography can be used to assess the extent of damage to the blood vessels, arteries and veins and even the capillary vessels of the eye. This technique is also used to examine the capillary vessels around the macula; however, new OCT techniques are already on the horizon that will allow the analysis of these vessels without contrast agents.
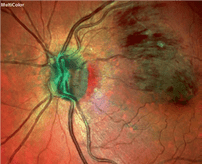
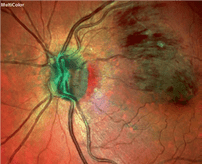
Fig. 2. Occlusion of a venous branch with a haemorrhage near the near the macula, which is used for reading.




Until recently, secondary diseases of diabetes on the eye could only be treated with laser. Often there was a loss of vision and completion of the treatment required numerous visits to the doctor. The laser continues to be a useful technique, but it has evolved so that nowadays the treatment is less traumatic (below the threshold of perception). Although it takes longer to show an effect with the new laser technique, it allows for the often long-term recovery of function (especially when the diabetes stabilises). Diabetic retinopathy (the medical term for diabetes-related eye disease) is often treated with eye injections. There are 2 major classes of drugs: Antibodies against VEGF (Lucentis, Eylea, Avastin) or corticosteroids (Ozurdex, Iluvien, Dexamethasone, Triamcinolone). Some of these drugs have not been tested in randomised trials and are not recognised by santésuisse, but they are all effective under certain conditions. Most require repeated injections into the eye to be effective and all require intensive medical care. In rare, more advanced cases, vitreoretinal surgery is the only option for preserving vision. Thanks to these treatments – and increasingly to their combination – it is possible to prevent vision loss and often even to reverse existing loss.
Through a combination of prevention and early detection with regular diagnostics and targeted therapy, most patients’ vision can be preserved. Visits to the ophthalmologist are unavoidable, but effective and efficient. The check-ups take very little time, so you can get back to your usual activities in record time.




![CH12768_BANNER-MANCASSOLA-980x180-EN[1]](https://rang-group.ch/wp-content/uploads/2021/05/CH12768_BANNER-MANCASSOLA-980x180-FR1.png?v=7646)





